18 min read
All About PCOS (Polycystic Ovary Syndrome)

They call it a string of pearls as if it were something desirable, beautiful, and exquisite. That was my first thought when I was initially diagnosed with PCOS at 17. Not as a possible PCOS diagnosis but as full-blown polycystic ovary syndrome that ticked all of the boxes – from very rare to absent periods, excess hair growth and belly fat, and ovaries that showed this characteristic string of "pearls". These were actually multiple immature follicles filled with fluid (quasi-cysts). This is where the name of the syndrome comes from: poly (meaning more) - cystic, aka multiple cysts that were never ovulated due to hormonal crossed wires in the body on one or both ovaries. I had (have) it on both.
It was a very confusing time for a young girl on her first visit to the gynecologist. This brings up mixed emotions even if everything is ok, with a mixture of shame and fear (of pain, judgement, being naked in front of a stranger... you name it), but finding out you have PCOS and being sent home with basically no instruction other than that you will be on birth control forever and will probably not be able to have children was quite defeating. I did try a few rounds of birth control. These did make my period come on time, but I wasn't feeling myself and did not recognise that passive girl. This was not my personality, and it was as if someone else moved into my body, someone I didn't know, so I stopped.
Women may feel fine on hormonal birth control and want to continue for years or decades. Kudos to them, but synthetic hormones were just not my cup of tea, glass of wine, or shooter of schnapps. Now looking at this scared 17-year-old at double the age (and then some more), it was all to be expected, really. PCOS is not entirely genetic, but it has a genetic component, and my grandma, mother, and sister have it too. I should have been prepared for the PCOS diagnosis, but I wasn't. And I was not prepared for no information whatsoever in an era when you still needed to ask people to get off the phone to use the Internet.
Twenty years later, I still don't appreciate sugar coating with the "string of pearls" talk. I understand it was not malicious, and it is just an aesthetic association. Still, it pisses me off because the acknowledgement of that string could have been used to help me take better care of myself, rather than to hang me out to dry with insufficient information.
We're here today so you don't need to feel as lost as I was on that table in a sterile, bare room, explaining my PCOS symptoms to a man who barely cared. I'm here to share what I've learnt from almost 2 decades of solo research on how to help my body. I'll go through some medical facts that we know, as well as the things we don't yet, and discuss medical and natural holistic ways to balance your hormones and make it easier for your body to return to balance. If you've already been diagnosed or have your suspicions and have googled around, you know that PCOS can't be permanently cured. Still, you can make good life choices in combination with supplements or medical options that will make the symptoms imperceptible and barely existent.
You may not have a PCOS belly, you may be overweight, you may not have problems getting pregnant, or you might need some extra help, but PCOS does not automatically mean infertility. Just ask my mom and grandma. We're all different, and we don't all manifest the same symptoms. It's more like a spectrum, but there are tendencies. So, let's dive in and start with the most obvious question: What is PCOS?
What is PCOS?
Polycystic ovary syndrome (PCOS) is not as rare as we may think, and there is no need to feel alone if you've got the condition. The WHO (World Health Organization) estimates that 6-13% of women of reproductive age are in your corner, and up to 70% are still undiagnosed. Some of these women have no apparent symptoms.

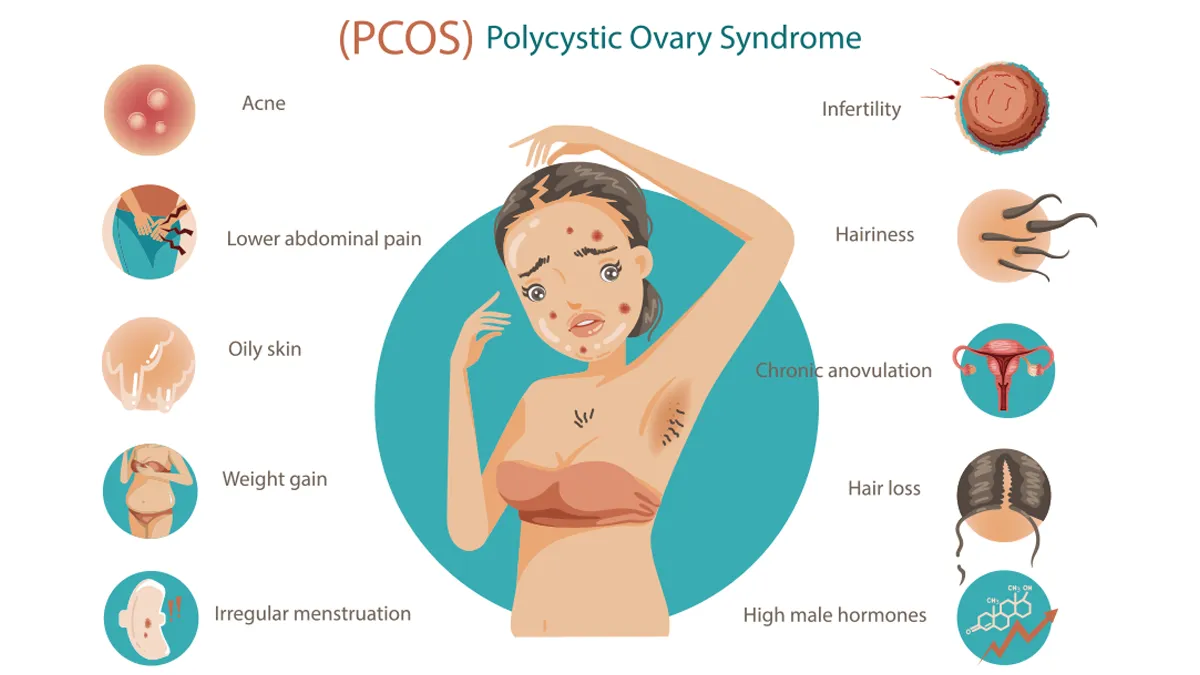
PCOS symptoms will usually start in adolescence, quite often soon after your first menstrual cycle. This is what happened to me after the first few normal-length cycles, which began to lengthen and eventually became absent. The signs of PCOS are not a simple list of symptoms, but may vary throughout life as the hormonal imbalance worsens or improves. PCOS is also considered to be the most common cause of anovulation (meaning no ovulation; you can get a cycle that can be anovulatory, where no mature egg is released) and a leading cause of infertility. Ovulating means releasing a mature egg to be fertilised. The name originates from the Latin "ōvum," meaning "egg," and the diminutive "ōvulum" (meaning "small egg"). If there is no ovulation, you can't get pregnant, because there is nothing for a sperm to fertilise. But PCOS is not the death blow for reproductive health.
Although chronic, PCOS can be significantly improved by decisions on your plate, how much you move your body, doing low to medium rather than high impact exercises (which will raise cortisol), and fertility treatments. These are quite successful if you choose to have children. No one is really sure what the cause of PCOS is, if it is mainly genetic or environmental, but it seems to be a little bit of both, with a powerful metabolic component. Issues like insulin resistance or type 2 diabetes can be caused by or cause PCOS. The body has a holistic approach even when we don't, and all things are interconnected in a self-amplifying loop. Fixing one problem might help you fix multiple others.
3 main symptoms for PCOS diagnosis
Irregular periods
This may vary from unusually long cycles (more than 35 days), fewer than 9 periods per year, months of skipping cycles, or even no cycles at all. Or you can swing the other way with very long periods. Suppose you have irregular periods, absent or anovulatory cycles. In that case, you will have trouble conceiving, because you can't count on the days when you're fertile, not knowing if the egg has been ovulated.
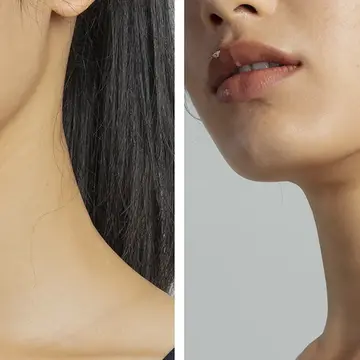
More androgens
High levels of these "male" hormones (women have some, but PCOS women have excess) may manifest as physical signs. For example, signs of high testosterone in a woman would be excess facial or body hair (hirsutism). This may also lead to increased hair loss.
Polycystic ovaries on ultrasound
One or both ovaries become enlarged and collect many fluid-filled follicles, up to 8mm (approximately 0.3in) that surround the immature eggs, placed around the edge of the ovary - this is the "string of pearls" we spoke of at the beginning.

You can and don't need to have all of these to be diagnosed. Two criteria fulfilled may be enough for a diagnosis, and you may also experience additional symptoms, such as:
- Gaining weight easily, especially visceral fat in the abdominal area, which makes PCOS present with an apple body shape
- Trouble losing weight with good lifestyle habits due to chronically elevated blood sugar, insulin, and insulin resistance (IR).
- Massive carb cravings result from unregulated blood sugar levels and poor signaling of satiety hormones.
- Very oily skin or adult hormonal acne
- Male pattern baldness or hair loss in general (usually due to excess androgens).
- Skin tags or dark, velvety patches (acanthosis nigricans) on the body folds indicate that you need to monitor your blood sugar and insulin levels.
Since there is a metabolic and inflammatory component to the condition, women with PCOS are more likely to have other health conditions, such as:
- type 2 diabetes
- hypertension (high blood pressure)
- high LDL ("bad") cholesterol and low HDL ("good") cholesterol
- heart disease
- endometrial cancer (cancer of the inner lining of the uterus)
- sleep apnea, a breathing disorder during sleep
- depression and anxiety
From this hormonal and metabolic roulette, I've gotten skipped to absent periods, the ovarian pearls, and a waist circumference larger than would be expected for my lifestyle, stubborn and unyielding even with daily exercise and calorie restriction (don't go down this rabbit hole; choose nutritious whole foods with a low glycemic index instead). You learn to live and love your PCOS belly once you realise it can be a bit better, but you'll most likely not have the body of a non-PCOS woman. The hormones have said their peace, and you will be mid-line heavier even if you're lean.
Keep in mind that the symptoms usually worsen as you gain more fat, because visceral fat is metabolically active and not inert like the jiggly belly fat. Belly fat, especially when located around vital organs, can contribute to further inflammation. I've been there and done that, with a long-term low-grade inflammation that resulted in autoimmunity, which I've now resolved by changing how I eat, sleep, and exercise rather than taking corticosteroids. It was my choice to take the harder route. Take the medicine if you need to and listen to your doctor. I'm just an (almost) middle-aged girl on the Internet telling her story, and I cannot make decisions for you.
I've also had some sleeping issues, which resulted in huge mood fluctuations to the point where I couldn't recognise or predict my own reactions in mundane situations, but this got better with taking a PCOS supplement containing Inositol and a tiny bit of melatonin. But we'll get to this in more detail later. Let's first go through what happens to get a diagnosis, for those of you who may suspect you have PCOS, especially for young girls, where a visit to the gynecologist still feels like a taboo. The doctor will not judge you, your body shape, body hair, or anything else you're worried about. They don't even care if you're currently bleeding, as they deal with bleeding all day long.
How is polycystic ovary syndrome (PCOS) diagnosed?
To start any kind of treatment, you really do need to get yourself checked out rather than self-medicating or popping unverified supplements like tic-tacs left and right. There is no one specific test for PCOS. Like, they just do this one thing and boom, you're diagnosed, but there are a few steps that are standard operating procedure in PCOS diagnosis. So how do they know if you have PCOS?
First, a doctor will ask about your medical history and family health history, particularly the female side of the family, to determine if there is a potential underlying genetic predisposition. They will ask you about your menstrual cycle, when you first got your period, and to provide them with the dates of the last few periods. You may also discuss the flow (heavy or light) and address any spotting or pain between cycles.
Then you'll get a physical exam, which will include looking for the physical signs of PCOS. Some of them we can see, like the dark velvety patches or skintags, excess hair, or hair thinning. For what we can’t see, you may get an ultrasound (over the belly for those who are not yet sexually active or transvaginal for those who are). The exam checks to see if your ovaries are enlarged or swollen and if you have the characteristic "pearls" on the edges. If doing an ultrasound, the doctor will also check the thickness of your endometrium (the lining of your uterus, or womb). It may be thickened if your period has been absent.
You may also undergo blood tests, including those to check your blood glucose, insulin sensitivity, or hormone levels, to confirm the diagnosis. Increased male hormones in a female would strongly suggest PCOS.
What causes PCOS?
I know this is not the answer any of us want to hear when we feel confused, lost, and don't know where to start, but the truth is - we don't know what causes PCOS ladies. This may not be all bad, not knowing. Once we know by the virtue of someone else's unshakable knowledge, we sort of just take what is offered and let go of the wheel of our own health. If we are still unsure, we go into Sherlock-mode, try to actually listen to our body, and find a way to help ourselves if there is consensus about the causes. This makes us do better and be better, learning and investigating, and much more likely to try lifestyle interventions than when handed a solve-all pill.
Although the cause of PCOS is not known, it does have at least in part a genetic component and often runs in families, with most women in the family having PCOS with a varying degree of symptoms.
Insulin resistance (IR) in PCOS
Many holistic and mainstream medicine perspectives repeatedly zoom in on and collect evidence for the metabolic components, such as insulin resistance, as a major trigger. This happens like this: You eat something, blood sugar rises, insulin comes in to mop up the excess blood sugar and take it directly to cells for energy production by burning with the presence of oxygen. This is why a walk after a meal, especially a carb-loaded one, is a great thing to do. Large muscles such as quadriceps (front thigh muscles) are always hungry for energy, and movement will reliably drop blood sugars that create such problems for PCOS women.
What the cells didn't want to absorb the insulin will store in fat cells to be used at a later date, once no food is coming in. That's why we like a good fast - to empty the old storage (glycogen from the liver and fat cells) now and then. Insulin is very serious about clearing sugar from the blood, because a lot of sugar circulating in the bloodstream is very dangerous. It is a neurotoxin and a great foundation for inflammation, which can damage the blood vessels and nerves. What happens in an insulin-resistant woman is that the cells become deaf to the insulin signal. This may be congenital or due to chronic abuse of processed carbs and overeating of carbs in general. Protein triggers only modest amounts of insulin, and fat triggers essentially none, so keto is sometimes recommended as a PCOS diet because it is a nutritional blueprint that goes low in carbs, but higher in protein and healthy fat. When the cells go deaf to insulin’s silent knock, the insulin starts yelling ever louder, rising two or three times above normal to deal with the same amount of sugar. The louder the insulin screams, the more the cells go deaf. If you had a constant noise buzzing in the background, you'd learn to ignore it as long as it doesn't change in pitch or volume. So less listening means more insulin noise and round and round we go, as rising insulin disrupts other hormones, such as enticing more testosterone production, starting the loop again.
All this starts making us gain weight, signaling an abundance of calories while we're still feeling tired and depleted because the cells (now half-deaf to insulin) can't use the energy around them. You simply cannot burn fat as long as insulin is high. It's like hitting the gas and the brake at the same time. You're going nowhere and might even damage the vehicle. So we get fatter, and the visceral fat joins the metabolic quire, creating inflammation that worsens the hormone signaling. Another loop.
How is PCOS treated?
How to cure PCOS permanently? This, too, is my great misfortune to inform you that basically, you can't. But, with the right choices - dietary, lifestyle, supplement, and well-calibrated medication and treatments - you can live your life symptom-free (which is the next best thing) and with no greater risk of severe comorbidities than anyone else without PCOS. My period is still not completely regular (as I chose no birth control), my body is still clutching to my ovarian pearls, and I am ok with my PCOS belly pouch now (most days), praising it and the uterus that lives there. I've managed all of my mood, sleep, and autoimmune issues quite well, if I may add. Minus a size larger pants and a period you can't count on, I'm quite fine.
PCOS treatments are not one-size-fits-all (it never is) and may take into consideration your age, the severity of symptoms, BMI, body composition, and your overall health. If you would like to become pregnant in the near future, this is also a factor and will exclude things like birth control.
If you are planning a pregnancy, the treatment may consist of:
PCOS diet
You may be advised to simply lose weight. This is very unhelpful because you can't lose weight as easily as someone without PCOS. Hearing this one advice repeated over and over again may only result in frustration, rather than a lower number on the scale. Calorie restriction does not work as well for us after the first few pounds, which are usually water weight, often tied to carbs and inflammation. In the long term, restricting all the time is unsustainable and will lead to overeating or massive weight gain once we stop restricting. We don't want to restrict and push the already unstable body into starvation mode, disrupting our hormones even more with the high cortisol that follows a prolonged deficit that the body views as stress. Starvation (not to be confused with a fast like 16:8 (fast 16: eat 8 hours) or OMAD (one meal a day)) is stress. We want to nourish our bodies with plenty of good foods and lose weight steadily rather than through crash diets.

When thinking about PCOS diets, think low carb. No need ot go radically low to ketogenic levels. Choose quality fats and protein sources (such as fish, lean meats, olive oil, nuts, and seeds) along with plenty of fresh vegetables (especially leafy greens and cruciferous veggies) and some low-glycemic-index fruits (berries and citrus fruits are great options). Eat carbs, but opt for whole foods that come with fiber, which slows down absorption and provides stable energy rather than a sharp blood sugar spike. Great choices include lentils, beans, sweet potatoes, and root vegetables (such as carrots, turnips, beets, and even regular potatoes). You can also have some rice, but try to make it integral rice or black wild rice, rather than plain white rice, and make sure to always eat your carbs with an addition of a salad or a good fat and protein source.
PCOS exercises
Diet alone is a significant piece of the puzzle, but it is incomplete without movement. The body was perfectly designed to move and burn the energy that it gets. Regular exercise, especially if you’re a student or have a sedentary job, will help you manage your weight, boost your mood, love your body, and lower blood glucose and insulin naturally. Very, very good news for us. The change will not happen overnight, but it will happen if you remain consistent.
Exercise for PCOS women does not necessarily mean joining a gym and doing Spartan sessions daily. Even small changes like leaving your car at home and going walking distances on foot rather than driving, gardening instead of plopping in front of the TV, or taking the stairs instead of an elevator daily make a difference. If you need something more structured, you'd be best off with medium-intensity training, such as bodyweight training, slow-weighted exercises with many repetitions, pilates, resistance bands, and perhaps short bursts of intensity, no longer than 30 seconds.
Avoid HIIT, as it can push your body into fight-or-flight mode and potentially exacerbate the issue. For cardio, do something steady like a longer swimming or cycling session. Walking uphill is always welcome. Find a hill or a mountain and conquer it. All of this can help your body use insulin more efficiently, lower blood glucose levels, and support ovulation.
Medication to help with ovulation
If you need a bit more of a push to ovulate a mature egg, there are medicines to stimulate ovulation, and they must be used under constant medical supervision, because they do have possible side effects and risks. They can increase the chance of a multiple birth (twins or more; are you ready for this?) and ovarian hyperstimulation, meaning the ovaries release too many hormones in the process of stimulation, where we want to coax them into giving us a healthy egg cell. Ovarian hyperstimulation can cause symptoms, such as belly bloating and pelvic pain, but most cases are mild and will not cramp your style (although they might cramp your belly). Keep in mind that most women with PCOS can get pregnant with help and have a healthy baby.
If pregnancy is not in plan for the foreseeable future:
Birth control pills may be added with synthetic hormones to control menstrual cycles, lower androgen levels, and reduce acne. Many women with very severe PCOS symptoms find using birth control very helpful. The plus is that you will be more protected from endometrial cancer, as the lining of the uterus will slough off in regular cycles. The steady controlled flow of hormones will greatly help those who suffer from adult acne, and may lessen your period pain if it is severe.
Diabetes medicine. It seems weird to use this before a diabetes diagnosis, but it is often used to lower insulin resistance in PCOS, and will sometimes be a part of the journey for women who wish to get pregnant with PCOS, as it will improve the chances of ovulation. Medications like metformin may also help reduce androgen levels, which can lead to less unwanted hair growth, reduced hair loss, and improved ovulation as the female hormones balance out in the absence of excess insulin. You may even shed a few pounds without the cravings that come with wild blood sugar fluctuations. A great way to improve your overall health and increase your chances of ovulation.
Inositol for PCOS?
If we are gonna go into supplements, there are a few deficits that usually come with PCOS, be it that we can't absorb them well, or that they get depleted through a higher inflammation profile in general. One of these superstars is the proven-to-work Inositol. You will hear it called vitamin B8, although it is not a vitamin but a sugar alcohol. It is naturally present in cells, and clinical studies suggest that inositol supplementation may help improve insulin sensitivity, reduce androgen levels, regulate menstrual cycles, and support ovulation. We know it under this common name, inositol, but there are actually 2 forms: myo-inositol (MI) and D-chiro-inositol (DCI), and although myo-inositol is the primary active form, studies have found the best effects when combining both in a 40:1 MI:DCI ratio, as this is also the natural physiological ratio in a healthy cell. Inositol for PCOS is also a very safe supplement that has absolutely none to very mild side effects.
Most people will tolerate it well, but if taken in excess (for example, ~12 g/day of myo-inositol, rather than the regular 2-4g/day), it may cause mild digestive distress, such as nausea, flatulence, diarrhea, but hey, so can too many apples. You should always tell your doctor, be it a GP or a specialist, about the medication and supplements you're using, and this is no exception. Regardless of being very safe, it still does affect insulin-sensitivity and blood-glucose control, and it can clash with anti-diabetes meds, meaning your blood sugar can go too low and you can experience the not very pleasant symptoms of hypoglycemia (low blood sugar).
Other useful supplements, or ideally nutrients we should focus on getting from whole foods, are:
- Magnesium
- Omega-3 fatty acids
- Zinc
- Berberine
- Vitamin D
- CoQ10
- Curcumin
- Vitamin B
- Probiotics
- Folate
- Melatonin
Conlusion
If there’s one thing I wish someone had told 17-year-old me, it’s that PCOS may shape my life in a way, but it does not get to define it. It was actually a blessing that taught me to take better care of myself. Yes, it’s frustrating, unpredictable, sometimes unfair, and often ignored by people who don’t live in this body - but it is also manageable, livable, and, with the right knowledge and medical support, something you can learn to work with, not constantly fight against.
PCOS is a lifelong relationship with and care of your hormones, your metabolism, and your mental health. There is no single diet, pill, supplement, workout, or doctor that will fix everything. There is only learning, trying, adjusting, and refusing to give up on your body, even when it feels like it has given up on you. Every walk after dinner, every balanced plate, every quality PCOS supplement, every boundary-protecting “no,” every tiny act of self-advocacy - they all accumulate into a better life and better health.
PCOS is not a failure of femininity. It does not make you less of a woman in any way, and although I wouldn’t choose it for myself had I been given the choice, it is not a curse. It is not the end of your fertility, beauty, or identity. It is simply a different road map - one that requires a little more navigating, a little more self-awareness, and a lot more kindness toward the person walking the path.
So wherever you are on this journey - newly diagnosed, deep in research mode, exhausted from trial-and-error, or already thriving, or are trying to help and support a woman you love in your life - you’re not alone. There are a lot of us out there ready to offer our story and what we’ve learnt so far, so that you don’t have to make all of your mistakes alone.






Leave a comment